Mental illness and substance abuse often travel hand in hand, a situation known as dual diagnosis. When both a mental health disorder and a substance use issue are present, each one can fuel the other—making recovery more complicated and increasing the chance of relapse.
Why Mental Illness And Substance Abuse Coexist
If anxiety or depression takes hold, reaching for alcohol or drugs may seem like the quickest way to ease the pain. Trouble is, that relief is temporary. Over time, substance use deepens mental health symptoms, which then drives more use. It’s a feedback loop that’s hard to break without the right help.
Consider these sobering figures:
- Over 3 million deaths around the world each year are tied to alcohol and drug misuse
- In the U.S., alcohol-related costs hit $249 billion annually
- Illicit drug use adds another $193 billion in economic burden
Yet only one in four people who need treatment actually receive it. For a closer look at these statistics and global trends, check out the WHO’s urgent scale-up report.
This guide will walk you through:
Coordinated care is essential to stop the cycle and boost long-term recovery.
Guide Roadmap
- Use a garden analogy to explain how mental health and substance use roots get tangled
- Lay out key risk factors and prevalence data side by side
- Compare standalone versus integrated treatment models in a clear table
- Share real-life case studies, including Tru Dallas Detox & Recovery Center’s approach
- Tackle common barriers and end with practical next steps
Key Takeaways
- Dual diagnosis means facing both mental health and substance use disorders at once
- Integrated treatment lowers relapse rates and addresses both issues together
- The high death toll and economic costs make coordinated care urgent
- Tru Dallas Detox & Recovery Center offers medically supervised programs designed for dual diagnosis
- You’ll learn core concepts, treatment options, and concrete strategies for recovery
Frequently Asked Questions
What Is Dual Diagnosis?
It’s the co-occurrence of at least one mental health disorder and one substance use disorder that requires combined treatment approaches.
Why Is Integrated Treatment Essential?
When care teams tackle both conditions at once, people experience fewer relapses and better long-term outcomes.
Understanding Dual Diagnosis With A Garden Analogy
Imagine a garden where every plant relies on the soil’s nutrients. In dual diagnosis, the roots of mental illness and substance use intertwine in that same soil. Pulling one weed won’t revive the whole bed if hidden roots still leech the life out of nearby plants.
You might focus on therapy to ease anxiety, yet prescription drug misuse goes unnoticed. Before long, reaching for a pill becomes a quick fix—and that relief loop only deepens both struggles.
-
Diagnostic Criteria
Presence of at least one mental health disorder and one substance use disorder within a 12-month window -
Common Pairings
- Anxiety and prescription drug misuse
- Depression and alcohol use
- PTSD and opioid dependence
Mental health professionals step in like gardeners running soil tests. They map out symptom severity alongside substance use patterns to avoid missing anything.
The DSM outlines that both conditions must appear within a 12-month timeframe. This formal check keeps misdiagnosis at bay and guides precise treatment from day one.
How The Garden Metaphor Explains Interaction
Think of a single diseased plant spreading fungus underground. Untreated depression works the same way—eroding coping skills and opening the door to alcohol misuse. Suddenly, cravings and dark thoughts feed each other, like vines choking the entire patch.
Globally, more than 1 billion people live with a mental disorder, and substance use often makes recovery a steeper climb. In fact, 727,000 suicides in 2021 underline how intertwined these issues can become. Read the full research about these intertwined outcomes
Integrated care is like tending to all plants at once rather than pulling a single weed.
Just as roots share water and nutrients, mental distress and substance cravings tap into the same neurochemical pathways. If one side depletes resources, the rest weakens—and relapse becomes far more likely.
Why Single Focus Treatments Fall Short
Pulling weeds from one corner while ignoring the overgrowth elsewhere leaves the garden full of weak spots. Similarly, treating only substance abuse or mental illness in isolation often leads to stubborn symptoms and relapse.
| Treatment Approach | Outcome |
|---|---|
| Single-focus treatment | Persistent symptoms and elevated relapse risk |
| Integrated Dual Diagnosis | Coordinated healing of mind and substance use relief |
Core elements of an integrated program work like drip irrigation, nourishing every root:
- Coordinated assessment and joint treatment planning
- Synchronized therapy sessions and medication management
- Ongoing monitoring to prune unhealthy patterns
These strategies yield:
- Better symptom management through combined therapies
- Lower relapse rates with sustainable holistic care
- An enhanced sense of wellbeing as mind and body strengthen together
For instance, pairing cognitive behavioral exercises with craving-management skills tackles both depressive thoughts and substance urges in one program. That parallel focus actually heals the entire root network.
Tru Dallas Detox & Recovery Center applies this method consistently.
Clinicians at Tru Dallas design treatment plans that untangle those roots through synchronized therapy and medication management. Patients learn to nourish mental wellness and manage cravings side by side—cultivating lasting resilience and recovery.
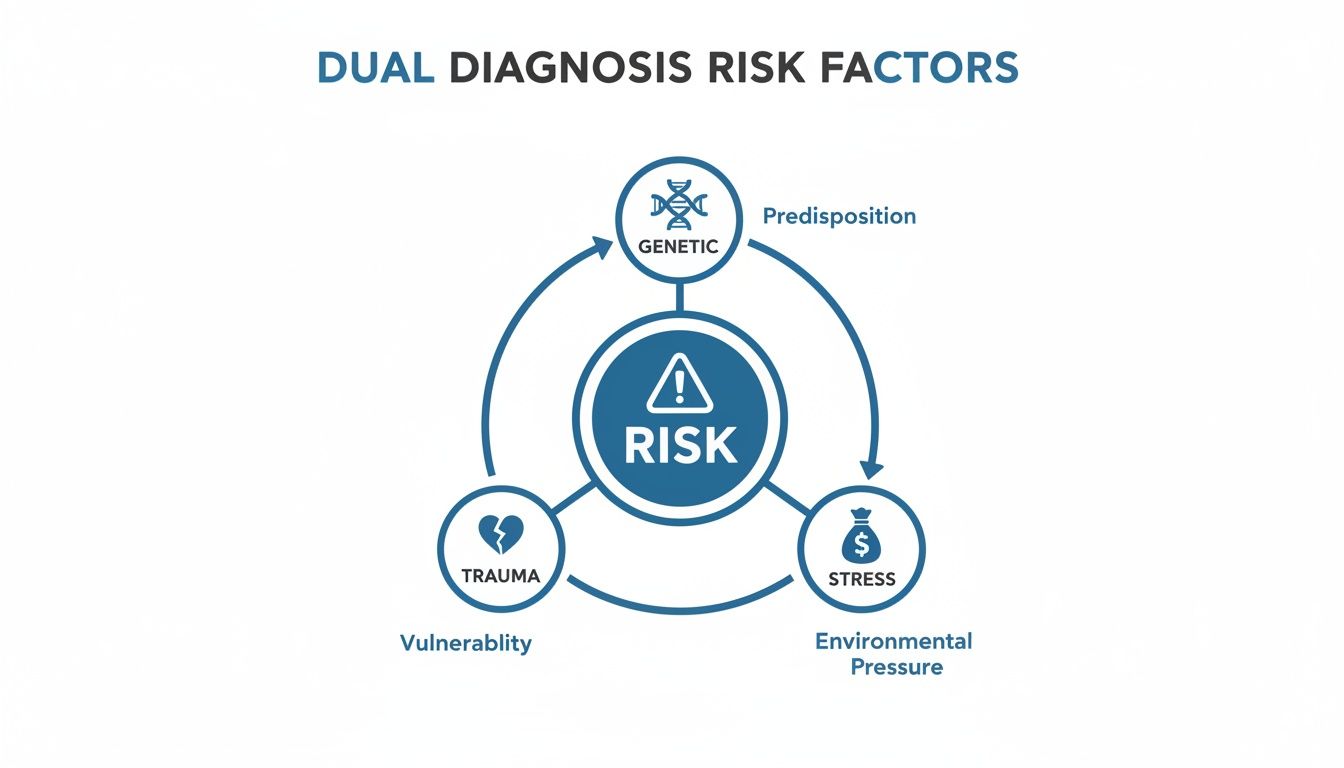
Risk Factors And Prevalence Of Dual Diagnosis
Mental health challenges and substance use often intertwine, each one making the other more intense. Think of it like two tangled roots underground—pull on one, and the other tightens.
Genetic predisposition can be that hidden fault line waiting for life’s tremors. If someone inherits a tendency toward mood disorders, alcohol or drugs may seem like the only way to steady the ground beneath them.
Early trauma—like growing up without consistent care—can leave a person searching for relief. Substances sometimes become a makeshift cushion against emotional pain.
- Genetic Predisposition: Inherited traits that increase vulnerability
- Trauma History: Early abuse or neglect disrupting coping skills
- Socioeconomic Stress: Financial strain heightening anxiety and substance use
- Environmental Influences: Peer pressure, community norms, and access to substances
Financial pressure—such as job loss or housing instability—often nudges people toward self-medication. Meanwhile, a neighborhood where drugs are easy to find can normalize misuse. Together, these factors raise the odds of developing a dual diagnosis.
Prevalence Rates Of Mental Illness And Substance Abuse
Below is a snapshot comparing how common substance use is among adults with different levels of mental health challenges.
| Group | SMI Illicit Drug Use | AMI Illicit Drug Use | Binge Drinking |
|---|---|---|---|
| U.S. Adults | 51.9% | 28.3% | 24.7% |
| Global Population | 31.2% | 18.5% | 15.1% |
These numbers shine a light on the overlap between mental illness and substance misuse, underlining why integrated care matters so much.
Targeted prevention can reduce the onset of dual diagnosis by addressing multiple risk factors early.
Certain groups—veterans who’ve seen combat or teens in high-pressure schools—face even greater risk. In low-income areas, limited access to therapy and higher substance availability only deepen the problem.
Prevention Strategies
- Early Screening: Incorporate mental health checks into routine doctor visits
- Trauma-Informed Support: Provide counseling right after adverse events
- Community Programs: Create safe spaces and peer support networks
When treatment addresses both mental health and substance use at the same time, relapse rates can drop by up to 40% compared to fragmented approaches.
Understanding these risk factors and prevalence trends helps shape focused prevention and early intervention. In the next section, we will explore evidence-based treatment pathways that build on these insights and pave the way for lasting recovery.
Regular screening in schools and primary care can catch issues before they spiral. And as policymakers collaborate to fund housing and regulate availability, communities grow stronger.
Evidence Based Treatment Pathways For Dual Diagnosis
When a mood disorder walks hand-in-hand with substance misuse, symptoms can spiral out of control. Integrated treatment tackles both challenges side by side, rather than in separate silos.
Research shows that integrated care models can lower relapse rates by as much as 40%. By weaving together therapy, medication, and peer support, people find a more balanced path to wellness.
This graphic lays out how genetics, trauma, and everyday stressors all collide to increase the risk of a dual diagnosis.
Core Modalities And Integrated Care
Picture a single care plan where your therapist and addiction counselor share notes and strategies. In a typical session, you might track your mood patterns one moment and practice coping drills for cravings the next.
- Joint therapy sessions that merge mental health techniques with addiction recovery skills
- Medical teams synchronizing medication dosages to ease withdrawal and stabilize mood
- Peer groups that reinforce coping tools for both anxiety and substance urges
Comparison Of Treatment Models
Here’s a quick look at how traditional and integrated programs differ:
| Aspect | Separate Treatment | Integrated Treatment |
|---|---|---|
| Therapy Sessions | Mental health and addiction care done in isolation | Single sessions combining CBT with recovery exercises |
| Medication Approach | Prescriptions managed by different specialists | Coordinated plans to minimize overlapping side effects |
| Support Services | Referrals to stand-alone peer groups | A unified network of dual diagnosis support |
| Outcomes | Higher relapse risk (up to 60% in one year) | 40% reduction in relapse, plus stronger quality of life |
By lining up every piece of care, integrated programs boost symptom control by roughly 25% and make clients feel genuinely supported.
"Coordinating care under one roof can cut relapse odds nearly in half."
Medication Management And Support
Medication in dual diagnosis often means a blend of antidepressants, antipsychotics, or MAT. Doses get fine-tuned to soften withdrawal while lifting mood.
Check out our guide to medication-assisted treatment strategies for dual diagnosis for detailed evidence on timing and dosage.
Peer Support And Community Healing
Nothing beats talking to someone who’s been in your shoes. At Tru Dallas, peer groups mix mental health check-ins with relapse prevention exercises in every meeting.
- Members swap tips for handling both panic attacks and substance cravings
- Facilitators step in at the first sign of distress to keep small issues from growing
- Community events introduce mindfulness, art therapy, and peer-led wellness workshops
Programs that include peer support see a 30% jump in long-term recovery success.
Real World Outcomes
When integrated dual diagnosis care clicks, stability and sobriety become more than just goals—they’re reality. Clients often report fewer hospital readmissions and a smoother emotional journey within a year.
- Faster mood regulation through combined therapy and medication
- Early intervention on triggers keeps relapse rates low
- Stronger self-confidence in managing co-occurring conditions
Next Steps For Recovery
If you’re facing both mental health challenges and addiction, look for a program where every part of your care is connected. Tru Dallas Detox & Recovery Center in Euless, TX offers medical detox, therapy, and peer support all under one roof.
Early involvement in an integrated program can boost long-term life quality by up to 50%. Reach out today to see how these evidence-based pathways can guide your recovery.
Real Life Cases And Personalized Care Approaches
Early Dual Diagnosis In A Young Adult
Ava, a 22-year-old college student, found herself trapped in a cycle of panic attacks followed by heavy drinking. Anxiety struck first, so she reached for a drink. The next morning, her nerves were raw, and the pattern repeated itself.
Her panic disorder and alcohol misuse formed a feedback loop—each problem fueling the other and making it impossible to see where one began and the other ended.
Early hurdles included her refusal to admit a substance issue and the stigma around mental health care. On her toughest nights, she even skipped therapy when cravings hit hardest.
- Early denial delaying a proper dual diagnosis
- Social isolation driving her back to alcohol
- Fragmented care forcing her to juggle multiple providers
You might be interested in reading inspiring recovery accounts in our addiction recovery stories collection.
Coordinated CBT And Medication
A turning point arrived once therapy and medication worked hand in hand. In cognitive behavioral sessions, Ava tackled both panic triggers and her urge to drink.
Low-dose SSRIs balanced her mood, so she could put coping strategies into practice. Keeping a joint journal for anxiety spikes and cravings proved eye-opening.
- Writing down anxiety and craving triggers every day
- Role-playing refusal skills in realistic scenarios
- Tweaking medication based on weekly reviews
This integrated path cut her binge episodes by 60% within three months, opening space for new, healthier routines.
Tru Dallas Detox Center Approach
Within the first 48 hours, Tru Dallas Detox Center runs a full dual diagnosis assessment. Clinicians watch for withdrawal symptoms and psychiatric signs at once, creating a single, unified care plan.
The image below illustrates how detox, therapy, and aftercare weave together:
Key elements include:
- Medical detox with medication-assisted treatment
- Integrated counseling combining CBT and relapse prevention
- Comprehensive aftercare plans involving peers and family
Aftercare features:
- Weekly follow-up calls to track progress
- Sober living referrals for stable housing
- Peer support group matching to maintain connection
Emotional Breakthroughs And Testimonial
A pivotal moment for many clients comes when belief in recovery outweighs fear of withdrawal. Sharing small victories in group sessions often sparks an emotional breakthrough.
“I didn’t think therapy could stop my panic until I saw how alcohol cravings and anxiety linked together. Here, I finally felt understood and supported.”
This honest insight shows how treating mental health and substance use as one condition validates everyone involved. It also proves that transparency and shared goals build trust and reduce isolation.
Overcoming Barriers And Common Misconceptions
Even though treatment for mental illness and substance abuse can turn lives around, myths still get in the way. Shame around stigma often makes admitting the problem harder than it needs to be. For instance, one person I worked with wouldn’t join a peer support circle until a friend shared their positive recovery story.
Worries about money can overshadow the value of early intervention. Sliding-scale fees or telehealth appointments often ease the financial pinch, making care more approachable.
Many also assume insurance won’t cover rehab. You can dive deeper into coverage and out-of-pocket costs in our detailed guide Does Insurance Cover Drug Rehab?
- Nearly 50% of individuals cite cost as a barrier to seeking integrated care
- Stigma remains a hurdle for 40%, leading to delayed intervention
- Telehealth services can increase access by up to 30%
“Understanding coverage options is a game changer for families navigating rehab,” says a Tru Dallas admissions counselor.
Addressing Fears Of Withdrawal
When someone imagines detox, they often picture painful symptoms. In reality, medically supervised protocols can significantly ease discomfort with targeted medications. This approach allows most people to get through the initial phase safely.
- Medication-assisted treatment that reduces cravings and nausea
- Round-the-clock monitoring by nurses and physicians
- Custom tapering schedules aimed at a gentler transition
- Peer-led sessions where former clients explain coping tactics
Cost And Coverage Misconceptions
It’s surprising how many centers offer sliding scales based on income. Telehealth also cuts travel time and related expenses, freeing up more of your day.
At Tru Dallas, we accept most PPO plans and guide you through pre-authorization. Our admissions team walks you through the fine print on deductibles and copays so you can focus on recovery.
- Double-check if we’re in-network before your intake appointment
- Ask about charity care slots or grant-funded programs
- Compare teletherapy rates against inpatient rehab fees
Preventing Dropout And Promoting Success
Keeping someone motivated through recovery takes a mix of clear goals, peer backing and real-time feedback. Early achievements, no matter how small, build confidence and momentum.
- Work with a clinician to set realistic recovery milestones
- Plug into a weekly support group or online forum
- Log progress in a shared journal or mobile app
Celebrating small victories early on makes a huge difference in sticking with treatment.
Starting care sooner rather than later can improve success rates by 60% compared to waiting for a crisis. With the right tools, realistic expectations and a support network, these common roadblocks don’t have to stand in the way of lasting recovery.
Stay connected to your community. Choose support over solitude.
Key Takeaways
- Treat mental health and substance use together through integrated dual diagnosis care for up to 40% fewer relapses.
- Combine therapy, medication management, and peer support to address interconnected symptoms holistically.
- Early screening, trauma-informed counseling, and community programs reduce the risk of dual diagnosis.
- Personalized treatment plans tailored to individual histories and goals improve engagement and outcomes.
- Removing barriers—like cost, stigma, and scheduling—ensures accessible, sustained recovery.
Frequently Asked Questions
What is dual diagnosis?
Dual diagnosis refers to the simultaneous presence of a mental health disorder and a substance use disorder that require coordinated treatment.
How does integrated care improve recovery?
By addressing both conditions at once, integrated care lowers relapse risk, enhances symptom management, and supports long-term wellness.
What should I look for in a dual diagnosis program?
Seek programs offering unified assessments, joint therapy sessions, coordinated medication management, and peer-led support.
How can families support a loved one?
Family involvement through education sessions, therapy participation, and ongoing encouragement strengthens adherence and outcomes.
Are there affordable integrated care options?
Yes—many centers offer sliding-scale fees, telehealth services, and insurance guidance to reduce financial barriers.